Can you give Topical Anesthetics for Corneal Abrasions?
Bottom Line Up Top: Short term (24-48hrs), appropriate use of topical anesthetics in patients with simple, uncomplicated corneal abrasions appears both safe and effective for pain management.
Clinical Scenario: A 40-year-old male presents after a blunt injury to the right eye with a nerf dart. He reports tearing and pain but no change in vision. He denies any contact lens use. You perform an extensive ocular exam. You instill 2 drops of topical tetracaine and the patient reports immediate relief. Visual acuity is 20/20 and you note a small oval shaped area of fluorescein uptake on the cornea outside of the visual axis with negative Seidel’s sign and no foreign body. After discussing the findings and management of a simple uncomplicated corneal abrasion with the patient and attending, the patient requests “something for pain” in addition to antibiotic eye drops. You consider whether it is safe to provide topical anesthetics to this patient for pain management at home.
What Your Gut Says: Don’t give topical tetracaine. The ophthalmologists don’t do it. Patients could develop keratitis, infections, scarring, sloughing, perforations, or non-healing from topical anesthetics.
What The Evidence Says: Many ophthalmologists caution against the practice of prescribing topical anesthetics. In general, they are the first to recognize and manage the complications related to abuse and misuse of topical anesthetics (Lee, 2019). Although we may not deal with these complications, they are serious. The evidence cautioning use against topical anesthetics includes only case reports and case series in which patients misuse and abuse topical anesthetics for weeks to months. Data supporting use of topical anesthetics mainly look at short term use (24-48hrs) in a controlled setting with a controlled amount. These high quality studies have not demonstrated adverse effects when topical anesthetics are used for short term periods in limited amounts. Further studies would be helpful in establishing safety. Exclusion criteria in these studies often include patients with penetrating injuries, large or complicated corneal abrasions/ulcers, prior surgeries, contact lens use, or presenting 36 hrs after injury.
Read More From our very own, Dr. Swami: The Safety of Topical Anesthetics in the Treatment of Corneal Abrasions
A Review Related Topics: Topical non-steroidal anti-inflammatory drugs for analgesia in traumatic corneal abrasions: Cochrane Review on Topical NSAIDs for corneal abrasions
References
Lee M, Gouin S, Driver T, Seitzman G. Cornea Specialists Do Not Recommend Routine Usage of Topical Anesthetics for Corneal Abrasions. Ann Emerg Med. 2019 Sept;74(3):463-6.
Verma S, Corbett MC, Patmore A, et al. A Comparative Study of the Duration and Efficacy of Tetracaine 1% and Bupivacaine 0.75% in Controlling Pain Following Photorefractive Keratectomy (PRK). Eur J Ophthalmol 1997;7:327–33.
Bisla K, Tanelian DL. Concentration-Dependent Effects of Lidocaine on Corneal Epithelial Wound Healing. Invest Ophthalmol Vis Sci 1992;33:3029–33.
Ball IM, Seabrook J, Desai N, et al. Dilute Proparacaine for the Management of Acute Corneal Injuries in the Emergency Department. CJEM 2010;12:389–96.
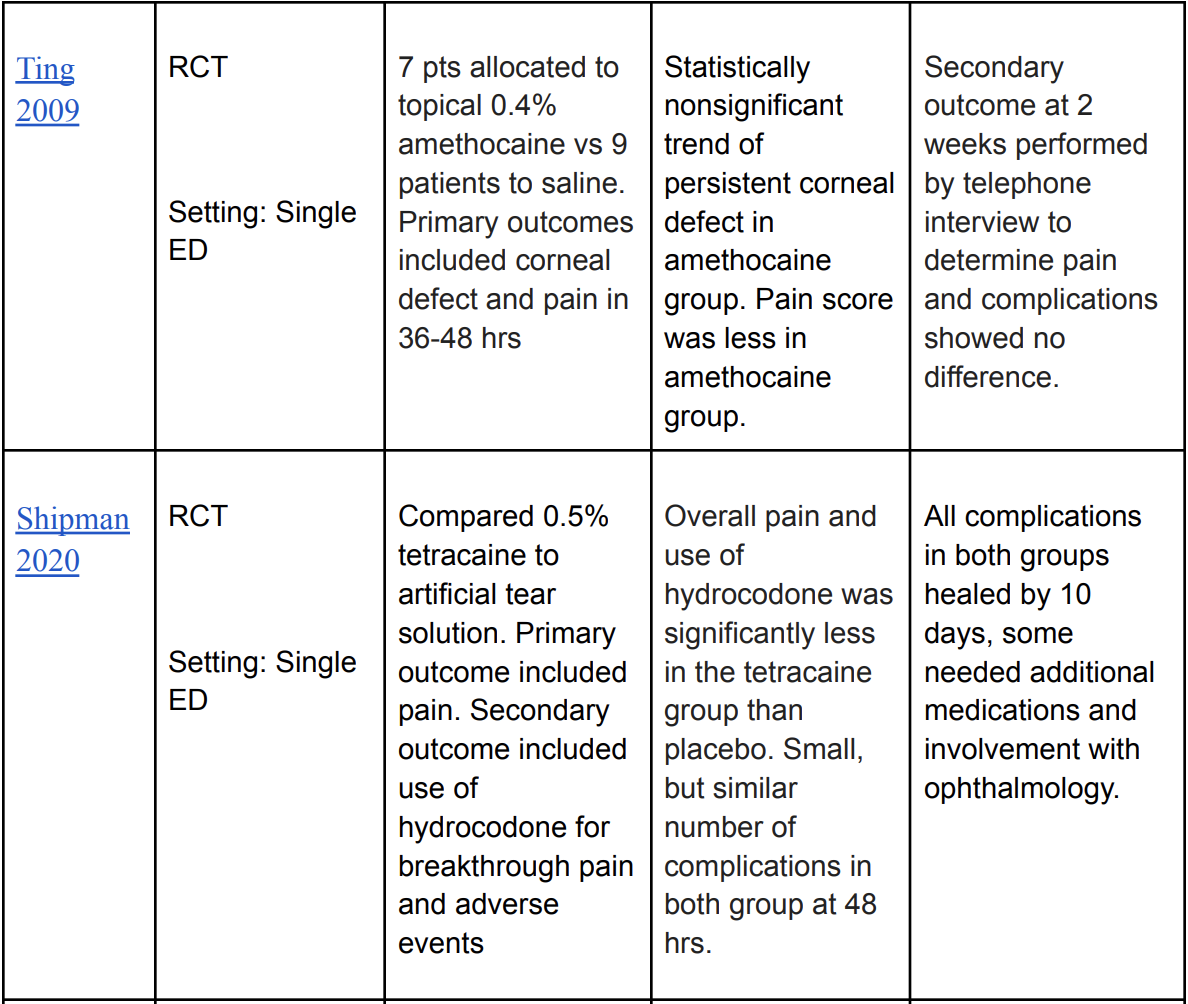
Ting JY, Barns KJ, Holmes JL. Management of Ocular Trauma in Emergency (MOTE) Trial: A Pilot Randomized Double-Blinded Trial Comparing Topical Amethocaine with Saline in the Outpatient Management of Corneal Trauma. J Emerg Trauma Shock. 2009 Jan;2(1):10-4
Shipman S, Painter K, Keuchel M, Bogie C. Short-Term Topical Tetracaine Is Highly Efficacious for the Treatment of Pain Caused by Corneal Abrasions: A Double-Blind, Randomized Clinical Trial. Ann Emerg Med. 2020 Mar;77(3):338-344
Waldman N, Densie IK, Herbison P. Topical Tetracaine Used for 24 hours is Safe and Rated Highly Effective by Patients for the Treatment of Pain caused by Corneal Abrasions: A Double-Blind, Randomized Clinical Trial. Acad Emerg Med 2014;21:374–82.
Brilakis HS, Deutsch TA. Topical Tetracaine with Bandage Soft Contact Lens Pain Control after Photorefractive Keratectomy. J Refract Surg 2000;16:444–7